Prostate cancer kills as many men as breast cancer kills women, so why is there less information about it in local health centres? KELLEY TANTAU continues her coverage of prostate cancer awareness during Blue September.
A little over a week ago, Barry Young was in a Thames cafe talking to a man about prostate cancer.
“I said to the bloke: ‘You’re about the age, have you had a check-up?’.
“He said: ‘No, I’ll never do that. If I get it, so what?’”
A number of reactions coursed through Barry’s body. As a former president of the New Zealand Prostate Cancer Foundation, and as a man who was diagnosed with the disease more than 20 years ago, his first thought was that the stranger was “stupid”.
“Second – I wondered if I should’ve done more to persuade him. Third – it was to, as I did, walk away from it and wonder what can you do?”
Barry tells it clearly. He has watched men die with the disease.
Every year, more than 4000 Kiwi blokes are diagnosed with prostate cancer and around 650-700 die from it.
Barry says he is “more than emotionally involved” because he was diagnosed when he was just 56.
He doesn’t want to tempt fate, but says “at this time” he is free of the cancer, and credits his positive outcome to good doctoring.
He was sent for a biopsy after his PSA test – a test that measures the amount of prostate-specific antigen in the blood – came back with a reading of 4.
“The first biopsy… nothing. But, being a good doctor, he said: ‘I really think we should do another’. I discussed it with my wife, Caroline, and she said: ‘Barry, they’re trying to tell you something’.”
Cells showing signs of change were found in Barry’s body, and eventually, he asked for a radical prostatectomy, a major operation which moves the removal of the entire prostate gland and surrounding lymph nodes.
“And I’m still here 25 years later.”
When he moved to Thames, Barry set up a group for all men’s cancers, but said he was now becoming “convinced” he needed to do more about prostate cancer.
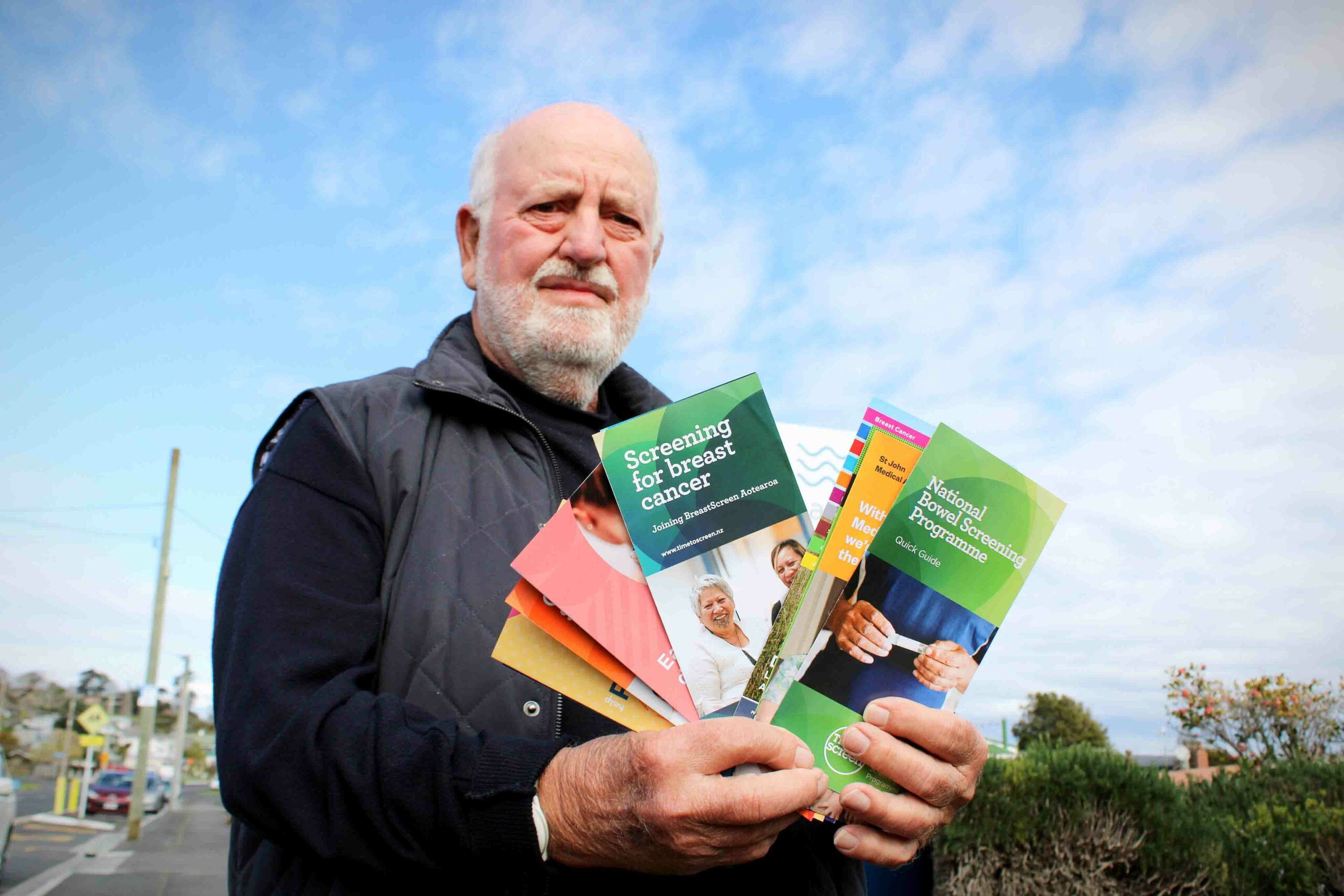
He visited the Thames Medical Centre and Te Korowai to look for information on the disease but couldn’t find any.
“I was in here [Thames Medical] some weeks ago, and went to the brochures, and while I was looking, one of the doctors came out and said: ‘Can I help you?” I said: ‘I’m looking for information about prostate cancer, and I can’t see any’.
“At neither place is there any information about prostate cancer. So, what is going on?
“Is this right through the country? If it is, it’s a bloody horror story.”
Paul Hayes, the NZ Prostate Cancer Foundation’s fundraising and marketing manager who manages Blue September, told The Profile the lack of availability of information on prostate cancer in GP and other health clinics was an ongoing issue.
“As far as we are aware, most Te Whatu Ora Health NZ regions do not routinely provide this information in either their hospital clinics or to primary healthcare clinics in their region.”
He said the Prostate Cancer Foundation had many different leaflets, posters, and other information tools that were available for both hospital and primary healthcare clinics to use, free of charge.
“The foundation has plans to distribute the education materials it produces on prostate cancer more proactively to relevant health clinics in the future. This is an expensive exercise and is one of the reasons why we run fundraising campaigns like Blue September to raise the funds that enable us to do this.”
Paul said even though prostate cancer was the most diagnosed cancer in New Zealand, little or no information about it was produced by Te Whatu Ora Health NZ or Te Aho O Te Kahu Cancer Control Agency.
The foundation “would really like” its educational brochures to be available in all relevant hospital clinics and in GP surgeries, but as a charity, it had not been in a position to send them out to clinics in an unsolicited manner.
Te Korowai Hauora o Hauraki told The Profile its brochure stands in its Whānau Health Centres were supplied by MediBoard, who also managed all of the content included on them.
A staff member checked the resources and confirmed there were none relating to prostate cancer; however, Te Korowai said its Whānau Health Centres would be “very happy” to make some prostate cancer informational resources available going forward.
Thames Medical Centre’s stands were also managed by MediBoard, and practise manager Carolyn Sara said various foundations often sent informaton and brochures, which the GP displays where suitable. A check of MediBoard’s downloadable brochures online did not show any prostate cancer options.
“You ask why this is not out and around, and I don’t know,” Barry says. “Women have done what they do for women’s health – breast cancer, cervical cancer – brilliantly, but prostate cancer… I think it’s largely because it’s to do with men’s sexuality. We’re bullet proof until it’s proved otherwise,” he says.
Barry encourages men to get check-ups from the age of 40. He also encourages them to ask for PSA tests.
“This, to me, is the most insidious fact that everyone needs to know: in its early stages, prostate cancer does not usually exhibit symptoms. So, men have it, and they don’t know they’ve got it.
“When symptoms do begin to occur, it is then usually too late for effective curative treatment. That’s the horror of this bloody thing.”
DETAILS: For more information on prostate cancer and Blue September, visit: prostate.org.nz