Health workers from across the Coromandel district protested in Thames on October 1, as Associate Health Minister Matt Doocey, Rural Communities Minister Mark Patterson, and a panel of local health experts fronted up for a national rural health roadshow.
The roadshow was the 12th such meeting to be held across the country since April.
Minister Doocey said the meetings were a chance for him to hear from those on the frontlines of rural health, and to understand how well the government’s Rural Health Strategy has been working since it was implemented last year.
“It is important that we shine a light on our needs and really drive the decision-makers forward about how we better support good health and social outcomes within our community,” he said.
Before taking questions, the Minister outlined the five priorities in the Rural Health Strategy – prioritising rural communities, improving preventative health interventions, increasing service availability, supporting access to distant services, and developing a valued and flexible workforce.
He also touched on the $164 million healthcare package in this year’s Budget, which will be used to strengthen nationwide urgent and after-hours care services.

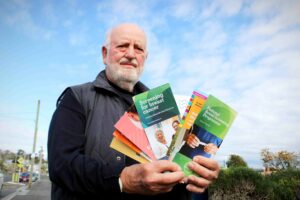
Ahead of the meeting, the Ministers toured Thames Hospital, where they spoke with New Zealand Nurses Organisation (NZNO) members who were picketing outside.
“[Minister Doocey] actually got out of his car and came and spoke to us… it feels like he listened to us,” Thames Hospital emergency department nurse and NZNO delegate Elizabeth Brundrit said.
The organisation has been fighting for extra nurses for some time, Elizabeth said, and the hospital is still understaffed despite being granted funding for 10 extra full-time nurses during last year’s hiring freeze by Te Whatu Ora Health New Zealand – only half of the numbers required.
“The word burnout, I’m hearing more and more and more,” Elizabeth said.
“We need more nurses on the floor… We have multiple shifts where we feel unsafe. We are concerned that we miss things, that there is a delay in getting the help and getting the treatment that [patients] need.
“And with any delay, there is going to be an increased risk.”
Elizabeth put her concerns to the panel during the meeting.
Panellist Rachel Swain, Te Whatu Ora Waikato’s operations director for community and rural health, acknowledged the stress the nurses were under.
She said she had just received approval for a flow nurse to help divert low-acuity patients from the emergency department, and also noted that data from the software used to predict hospital staffing needs had been resubmitted for further review.

Several other issues were also raised during the meeting.
Telehealth was a major topic, as local providers questioned the Minister about the government’s recently-announced Digital 24-7 initiative.
Minister Doocey cautioned that telehealth was not to be seen as a “silver bullet”, and was intended to complement existing in-person services by providing choice and convenience.
Another talking point was the need to increase the available workforce, and make it easier for health professionals to live and work in the area.
The overarching theme of the questions put to the Minister though, was whether local health services would be tailored to the region’s unique geography and demographics, and allow for sufficient input from local providers during the development process.
“Our community has been working for over 50 years to develop its own infrastructure to enable the resilience of our community because we are a land island, often closed off in Thames and Coromandel by the slips,” Dr Kate Armstrong from the Colville Project said.
Te Korowai Haora o Hauraki chief executive Tammy Dehar said any policies needed to consider the needs of the whole community, including both the over-65s and the growing numbers of youth.
Minister Doocey said the government was open to ensuring decision-making in the sector came from as close to the frontline as possible.
“You know your communities, you know the uniqueness of it, and also the need, because quite often you know the people in your community you need to work with as well,” he said.
“The problem we had with centralising the health system, I think it was quite dangerous in a mental health context, because what works for, say, middle-aged Pākehā dairy farmers where I live in North Canterbury could be quite different than [for] young Māori in the Coromandel.”